State Health Benefit Plan (SHBP)
The State Health Benefit Plan (SHBP) is established for the benefit of school districts and other governmental employers by the Georgia legislature. SHBP operates through the Georgia Department of Community Health (DCH). SHBP and DCH determine the plan design, the monthly premiums, and the network providers. Effingham County Board of Education provides payroll deduction for your premium along with other administrative support. A Decision Guide is available for plan details, and the monthly premiums are available in the Premiums section.
You may choose between Anthem and UnitedHealthcare for your health plan coverage. Anthem offers four plan options: three HRA plans and one HMO plan. The HMO plan option provides in-network coverage only, and requires copays for many services. UnitedHealthcare offers an HMO similar to the Anthem plan, along with a High Deductible Health Plan (HDHP). The HDHP has the highest deductible and out-of-pocket costs, but the lowest premiums.
The Anthem plans include Gold, Silver, and Bronze HRA plan options, and an HMO plan option. On the HRA plan options, most services are subject to a deductible and there are no copays. After you meet your in-network deductible, you pay coinsurance up to the out-of-pocket maximum. For prescription drugs, you pay a percentage of the retail cost. The HRA plans include a plan-funded Health Reimbursement Account to reduce / offset your deductible and pharmacy expenses (unused balances carry forward into new plan years). Preventive care is covered at 100% in-network before the deductible.
The HMO plan option has the lowest deductible out of all plans, but provides in-network coverage only. Some services (office visits, ER visits, and prescription drugs) are covered at 100% after a copay. For most other services, you are responsible for a deductible and coinsurance until you meet your out-of-pocket maximum. Please be aware that copays do not count towards your deductible. Preventive care is always covered at 100% before the deductible.
The UnitedHealthcare plans include an HMO option and a High Deductible Health Plan (HDHP) option. This HMO plan has the same benefits as the Anthem HMO, but utilizes the UHC network.
The HDHP plan has the lowest premiums, highest deductible, and highest maximum out-of-pocket costs. All services, including pharmacy, are subject to the deductible and coinsurance, and there are no copays with this plan. Once you meet your deductible, you pay coinsurance until you satisfy the out-of-pocket maximum. As with the other State Health plan options, wellness incentive points can be earned by High Deductible Health Plan members. You are eligible to open an HSA if you enroll in the State Health Benefit Plan (SHBP) High Deductible Health Plan (HDHP) and do not have other coverage through 1) your spouse’s employer’s plan, 2) Medicare, or 3) Medicaid. The HSA is not set up through the district and must be established separately.
Effingham County Schools contributes $1,885 per employee per month towards your medical coverage. This is an annual employer contribution of $22,620.
Transfers from Other Georgia Systems
- If you transfer from another Georgia system, you must retain your current medical coverage for the remainder of the calendar year.
- No changes are allowed to your SHBP coverage until the next Open Enrollment period, unless you have a Qualifying Life Event (QLE).
Medicare
For active employees with spouses that are enrolled in Medicare and not disabled, SHBP is primary. The spouse is not required to elect Part B (medically necessary services such as outpatient care and preventive care) until the active employee retires. However, the spouse will automatically receive Part A (hospital insurance).
Please note: As a new hire, you have 31 days from your date of hire to enroll in your medical benefits.
|
Anthem HRA Plan - Gold In | Out |
Anthem HRA Plan - Silver In | Out |
Anthem HRA Plan - Bronze In | Out |
Anthem / UHC HMO Plan In (No Out-of-Network Coverage) |
UHC HDHP Plan In | Out |
|
|---|---|---|---|---|---|
|
Deductible
|
|||||
|
You
|
$1,500 | $3,000 | $2,000 | $4,000 | $2,500 | $5,000 | $1,300 | $3,500 | $7,000 |
|
You + Child(ren) / Spouse
|
$2,250 | $4,500 | $3,000 | $6,000 | $3,750 | $7,500 | $1,950 | $7,000|$14,000 |
|
You + Family
|
$3,000 | $6,000 | $4,000 | $8,000 | $5,000 | $10,000 | $2,600 | $7,000|$14,000 |
|
Medical Out-of-Pocket Max
|
|||||
|
You
|
$4,000 | $8,000 | $5,000 | $10,000 | $6,000 | $12,000 | $4,000 | $6,450 | $12,900 |
|
You + Child(ren) / Spouse
|
$6,000 | $12,000 | $7,500 | $15,000 | $9,000 | $18,000 | $6,500 | $12,900|$25,800 |
|
You + Family
|
$8,000 | $16,000 | $10,000 | $20,000 | $12,000 | $24,000 | $9,000 | $12,900|$25,800 |
|
Coinsurance (Plan Pays)
|
85% | 60% | 80% | 60% | 75% | 60% | 80% | 70% | 50% |
|
HRA Credits
|
|||||
|
You
|
$400 | $200 | $100 | N/A | N/A |
|
You + Child(ren) / Spouse
|
$600 | $300 | $150 | N/A | N/A |
|
You + Family
|
$800 | $400 | $200 | N/A | N/A |
|
Medical
|
|||||
|
ER
|
Coins after ded | Coins after ded | Coins after ded | $200 copay | Coins after ded |
|
Urgent Care
|
Coins after ded | Coins after ded | Coins after ded | $35 copay | Coins after ded |
|
PCP Visit
|
Coins after ded | Coins after ded | Coins after ded | $35 copay | Coins after ded |
|
Specialist Visit
|
Coins after ded | Coins after ded | Coins after ded | $45 copay | Coins after ded |
|
Preventive Care
|
100% | None | 100% | None | 100% | None | 100% | 100% | None |
Pharmacy Benefits
CVS Caremark is the pharmacy vendor for all medical options.
- For the HRA, you pay a percentage of the cost subject to a minimum and maximum per prescription.
- For the HMO plans, prescription drugs are covered at 100% after a copay at participating pharmacies.
- For the High Deductible Health Plan, prescription drugs are subject to deductible and then coinsurance, similar to other medical services.
The pharmacy costs are included in your out-of-pocket maximums, and a mail order benefit for a 90 day supply is also available. Additional details are located in the State Health Benefit Plan Decision Guide.
|
Retail Pharmacy |
Anthem Gold HRA |
Anthem Silver HRA |
Anthem Bronze HRA |
Anthem/UHC HMO |
UHC HDHP |
| Tier 1 |
15% Min $5 Max $10 |
15% Min $5 Max $10 |
15% Min $5 Max $10 |
$5 copay |
Coinsurance after deductible |
| Tier 2 |
25% Min $55 Max $85 |
25% Min $55 Max $85 |
25% Min $55 Max $85 |
$55 copay |
Coinsurance after deductible |
| Tier 3 |
25% Min $85 Max $130 |
25% Min $85 Max $130 |
25% Min $85 Max $130 |
$95 copay |
Coinsurance after deductible |
Disease Management Program
Managing chronic health conditions can be challenging, but the State Health Benefit Plan (SHBP) offers support to help ease the burden. Through SHBP's Disease Management Programs, you have access to valuable resources designed to help you better manage conditions like diabetes, asthma, coronary artery disease, and addiction. These programs provide personalized care and guidance, ensuring you stay on track with your treatment while also lowering your healthcare costs.
Certain drug costs are waived if SHBP is primary and you actively participate in one of the Disease Management Programs for diabetes, asthma, coronary artery disease, and/or medications for additction treatment.
To enroll in SHBP’s Disease Management Programs, you can access your SHBP enrollment portal online at mySHBPga.adp.com or contact SHBP Member Services at (800) 610-1863 for assistance.
Telemedicine
The medical plans include a telemedicine benefit through LiveHealthOnline, which allows you to speak to a participating doctor from home or work through your smartphone, tablet or computer 24 hours a day / 7 days a week.
You must use in-network providers for coverage to apply. HMO members pay a copay and HRA members pay coinsurance for telemedicine. High Deductible Health Plan members can access this benefit subject to the health plan deductible.
Consider utilizing your telemedicine benefit for non-complex medical conditions. Download the LiveHealth online mobile app (Anthem participants) or the Virtual Visits mobile app (UHC participants) for convenient access to telemedicine visits.
More information is available under Resources.
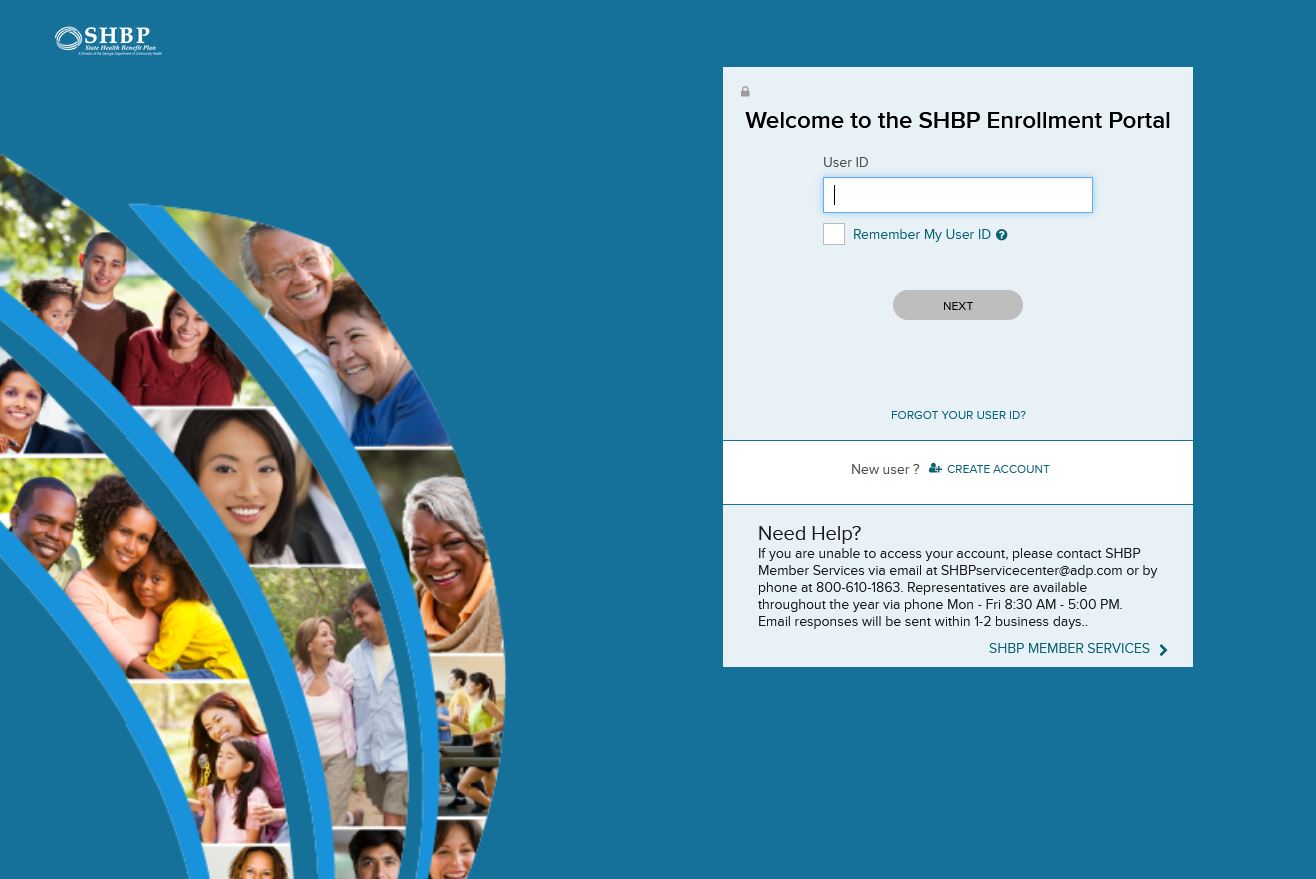
Enrollment - ADP Portal
How to complete your State Health Benefit Plan (SHBP) Enrollment through the ADP Portal.
- Access https://myshbpga.adp.com/shbp to review your health coverage elections. Your registration code is "SHBP-GA."
Once registered, you should:
-
Verify your address
-
Verify your coverage tier (you only, you & spouse, you & child(ren) or you & family)
-
Verify your dependents
-
Answer the Tobacco Surcharge question
-
Make sure you print your confirmation, write down the confirmation number, or save an electronic copy
Dependent Verification
- If you wish to add dependent(s) (spouse and / or children) to your health plan, ADP will contact you (by mail and email) to request appropriate verification documents. If you do not receive the request, contact SHBP directly to have the request sent to you. They can be reached at (800) 610-1863.
- The communication from ADP will include a personalized fax cover sheet with a bar code that must be used when submitting documentation.
- Appropriate documentation must be attached to the fax cover page and provided by the deadline set by ADP.
- Non-verified dependents cannot be reinstated until the next open enrollment period and would require appropriate documentation.
- Additional information can be found on the SHBP website.
Additional Resources
Go Online for More Resources
Access the two following plan websites to locate the participating providers and to find health and wellness tools, plan details, and to print ID cards.
Anthem
Select "Find Care' from the Main Menu and then follow instructions to find a doctor.
UnitedHealthcare
Select "Search for a Provider" under the Benefits drop down. Select "Choice HMO" or "HDHP with HSA" and follow the search instructions.
Other Medical Plan Options
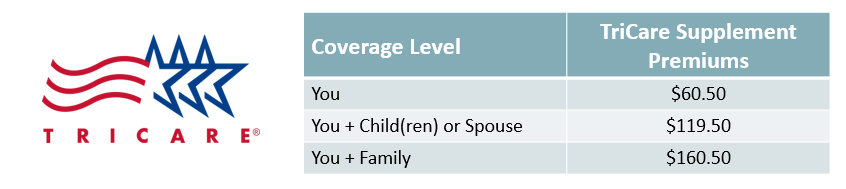
TRICARE Supplement Plan
The TRICARE Supplement Plan is available for retired military employees, and is a supplement to your current TRICARE benefits. The plan provides reimbursement of copays and other medical expenses associated with your current TRICARE plan. Additional information can be found here.
PeachCare for Kids
The state of Georgia offers an affordable health insurance program called PeachCare for Kids. This plan provides healthcare, dental, and vision benefits for children up to age 19. To learn if you are eligible, and to obtain benefits, cost, and application information, click here.

Shared Savings Program
Classified Employees May Be Eligible to Receive an Extra $3,000 Per Year.
Our Shared Savings Program allows you to receive a cash incentive to explore other healthcare options available to you. If you are a Classified Employee currently enrolled in medical coverage through State Health Benefit Plan - and you decline coverage during Annual Enrollment - you may be eligible for the Shared Savings program. Consider your options:
- If your spouse has coverage available, you may be eligible to enroll in their employer’s plan.
- If you are under age 26, you may be eligible to be covered under your parent’s benefit plan.
- Some employees may be covered both at the district AND under their spouse’s plan. If you are in this situation, you may not be receiving the full benefit for the money you are spending.
You are eligible for the Shared Savings Program, if you:
- Are a Classified Employee currently enrolled in the District’s medical plan
- You decline medical coverage during annual enrollment; and provide confirmation of declining
- You provide proof of other insurance for everyone in your “tax family” (who you claim as deductions for the current tax year)
- Return the enrollment form during Open Enrollment
If you meet the above criteria, you are eligible to receive a cash bonus of $3,000 per year, paid in equal monthly installments. Under IRS requirements, your cash bonus is considered taxable income.
Enrollment is only allowed during Open Enrollment or with a Qualifying Life Event. When you enroll in the Shared Savings program as a result of a QLE, the credit will be pro-rated. If you waive coverage from the District, you may re-enter the plan during the next annual enrollment period or if you have a Qualified Life Event, such as:
- You lose eligibility for other coverage due to the loss of spouse’s coverage
- Loss of your other group coverage due to divorce, termination, or a reduction in hours
- Marriage
- The birth or adoption of a child